
Different medications may be needed to help people with diabetes achieve target health goals. Here are the most common medications used in diabetes management.
Previously, I’ve covered several “Diabetes F-words”. The next one is formulary, better known as medications.
Since your diabetes diagnosis you have probably heard more about medications than you care to admit. However, despite all that you’ve heard, you may still have some questions. For example:
-
Why were you started on metformin?
-
Why was another medication added after several months even though your A1c had come down a little?
-
What’s the difference between the various pills?
-
How many pills can you safely take?
And so on and so on…
Well let’s start from the top.
People With Type 2 Diabetes
You were likely given a diagnosis of type 2 diabetes after having two fasting blood sugars over 125 mg/dL, an A1c (short for HbA1c) > 6.5%, a random blood sugar >200 mg/dL or some combination of these.
Once diagnosed the goal is to see if glycemic targets can be reached with diet and exercise (previously discussed). If the target A1c of <7% was not achieved or started to rise over time you were likely started on pills. According to the American Diabetes Association (ADA) and the American Association of Clinical Endocrinology (AACE) the medication recommended to be started first is Metformin.
That being said, let’s take a look at Metformin, along with the other medications that can be prescribed to assist with getting your blood sugar to target, and how they work.
Common Diabetes Medications
Here are the most common medications used for type 2 diabetes, common brand-names you may hear from your doctor, how they work, side effects, helpful suggestions and some cost info.
Biguanide - Metformin
- How it works: Lowers glucose production in the liver, reduces sugar absorption through intestines into bloodstream, increases insulin sensitivity.
- Side effects: Nausea, diarrhea
- Suggestions: Take with meal, try extended release (XR or ER)
- Cost if not insured: $4
Sulfonylurea (SU) - Glipizide/Glyburide
- How it works: In type 2 diabetes, makes the pancreas produce more insulin.
- Side effects: Can cause low blood sugar (hypoglycemia) if taken without eating
- Suggestions: Take with meal
- Cost if not insured: $4
Thiazolidinedione (TZD) - Actos
- How it works: Increase body's insulin sensitivity.
- Side effects: Can cause weight increase around the waste (more side-effects found here)
- Suggestions: Ask provider before taking if you have heart disease
- Cost if not insured: $$ (varies by pharmacy - find better prices from GoodRx)
Secretagogue (MLD) - Prandin
- How it works: In type 2 diabetes, forces the pancreas to release more of its produced insulin.
- Side effects: Can cause low blood sugar (hypoglycemia) if taken without eating
- Suggestions: Take with meal
- Cost if not insured: $$ (varies by pharmacy - find better prices from GoodRx)
SGLT-2 Inhibitor - Canagliflozin (Invokana), Dapagliflozin (Farxiga), Empagliflozin (Jardiance)
- How it works: Prevents kidneys from re-absorbing glucose so the body can dispose of more glucose through the urine.
- Side effects: UTIs, yeast infections, possible DKA.
- Suggestions: Seek care if you are sick (nausea, vomiting, abdominal pain) or planning a surgery
- Cost if not insured: $$$ (very high average price - find lower prices for each from GoodRx)
DPP-4 Inhibitor (Gliptins) - Januvia, Tradjenta
- How it works: Increases insulin in response to food by blocking an enzyme that destroys the hormone incretin.
- Side effects: Joint pain, mild flu symptoms, kidney problems
- Suggestions: Do not take if you are taking a GLP-1
- Cost if not insured: $$ (high average price - find lower prices for each from GoodRx)
GLP-1 RA - Rybelsus, Trulicity, Victoza, several others
- How it works: Enhances insulin release, reduces glucagon response, decreases appetite.
- Side effects: Nausea, gastrointestinal effects
- Cost if not insured: $$$ (very high average prices across several brand-name options - find lower prices for each from GoodRx)
Alpha Glucosidase Inhibitor (AGI) - Acarbose, Miglitol
- How it works: Blocks the breakdown of starchy foods and slows absorption of some forms of sugar.
- Side effects: Mild, temporary digestion issues
- Suggestions: If you experience low blood sugar, treat with dextrose-based glucose tabs/gel
- Cost if not insured: $ (lower average cost than many other diabetes medications - find lower prices for these from GoodRx)
* Please note: this list does not include all type 2 diabetes medications.
Type 2 Diabetes Management Decision Tree
Now that you have an idea about the various medications, let’s look at how decisions are usually made on which medications to add to Metformin and when to add them.
Medications are usually added if A1c has not reached target of 7.0% or less.
When adding medications your provider takes into consideration whether or not you have heart disease or chronic kidney disease. They also think about whether you have experienced hypoglycemia in the past or if you could possibly be at risk for it in the future.
If your weight is not at goal and you would benefit from losing weight they will likely add a medication that will help you with that. And lastly, if you are having difficulty covering the cost of your medications, that could also be a reason that they prescribe a different medication (see algorithm below).
Next--When to add another medication to Metformin. In most cases, you will have an A1c done every 3-4 months. At that time, if the A1c is not within target, a second medication will be started based on the factors previously discussed. You will then be given another 3-4 months to see if these 2 medications, along with diet and exercise are enough to bring your A1c within target. If not a third medication will probably be added. In the next 3-4 month interval if A1c is still not at goal (often if above 8.5%) long-acting insulin will be started.
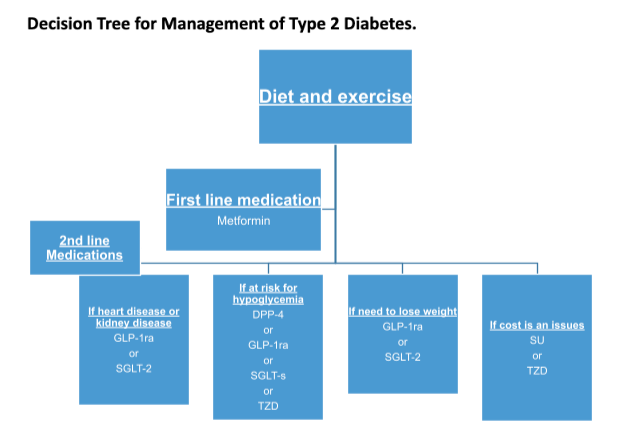
*Based on ADA algorithm. Standards of Medical Care in Diabetes—2020 Abridged for Primary Care Providers
People With Type 1 Diabetes
Insulin is your main formulary item. Because people with type 1 diabetes don't produce any insulin naturally, insulin needs to be self-administered. Here's a list of all types of insulins, delivery methods, and how to find out your best options.
For those of you with type 1 diabetes, keep in mind that sometimes one of the above medications, labeled for type 2 diabetes management, may sometimes be prescribed to assist you in getting to goal as well. The medications that are usually considered are GLP-1 Receptor Agonist (GLP-1 RA) and sometimes and SGLT-2 Inhibitor (SGLT-2 I) for those who are overweight. This is often referred to as off-label use, meaning that insulin is always the recommended medication for persons with type 1 diabetes, but occasionally your provider may try adding something to see if they can assist you with attaining your A1c targets.
Conclusion
So you see, there is thought given to adding diabetes medications. The goal is to get the A1c to target in order to prevent adverse effects due to high blood sugar. If at anytime you are experiencing side effects from your medications or have issues with affording them, be sure to discuss with your healthcare provider.





