
Accuracy is a range, not an exact number. Ginger Vieira explains the variables that apply to all FDA-approved glucose meters.
Every time you check your blood sugar using an at-home glucose meter the results you’re seeing on your screen is not the exact amount of glucose in your bloodstream.
This can be a little alarming if it’s the first time you’ve heard this because people with diabetes are making critical decisions based on that number. The fact is that getting an exact measurement of your blood sugar isn’t as easy as it seems.
In this article, we’re going to take an in-depth look at the standards glucose meters must meet in order to acquire the FDA’s approval for diabetes care -- and why your blood glucose meter’s results are within a range instead of an exact measurement.
Is Diathrive's glucose meter accuracy as good as other meters?
The answer is yes. Actually, it’s among the most accurate meters that are FDA-approved and available on the market, even when compared to meters from the top pharmaceutical giants.
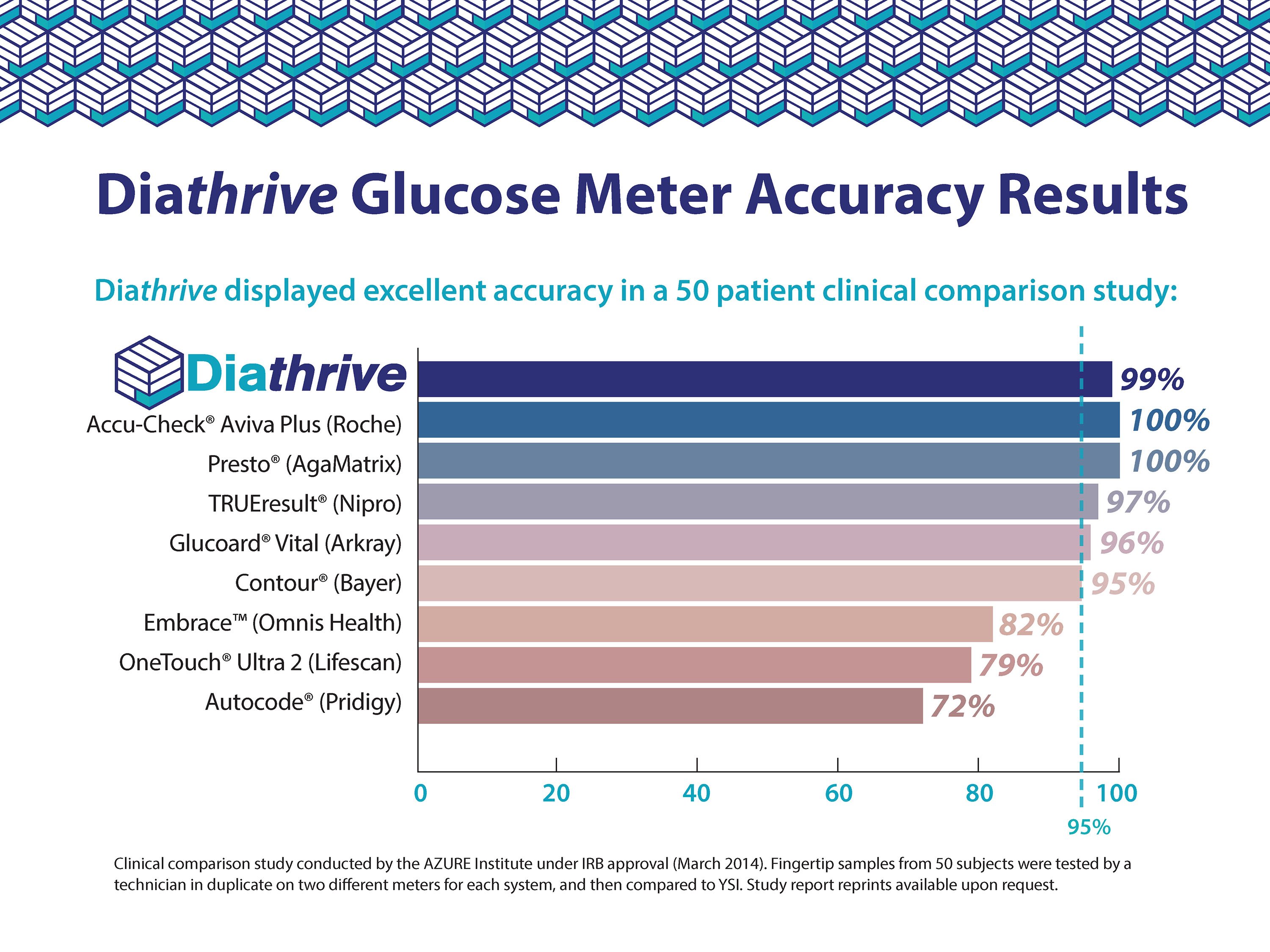
At only $10 for the actual glucose meter and 16 cents per strip -- all without a prescription, health insurance, or shipping costs -- Diathrive’s glucose meter is also the most affordable on the market.
How accurate is the average FDA-approved glucose meter?
When it comes to FDA-approved glucose meters, a meter must meet certain blood glucose meter accuracy standards similar to those set by the International Organization for Standardization (ISO Standard), but it’s important to know that accuracy does not mean an exact measurement.
Every glucose meter and blood glucose monitoring system available for sale in the United States today is approved by the Food and Drug Administration (FDA) and is required to be within 15 percent of “lab value” glucose readings 95 percent of the time, and within 20 percent of "lab results” 99 percent of the time (these ranges of inconsistency are called variance).
Diathrive’s meter is within 15 percent of “lab value” 99 percent of the time!
Take a look at how the blood glucose value on your glucose meter is actually giving you a number within a range rather than an exact number.
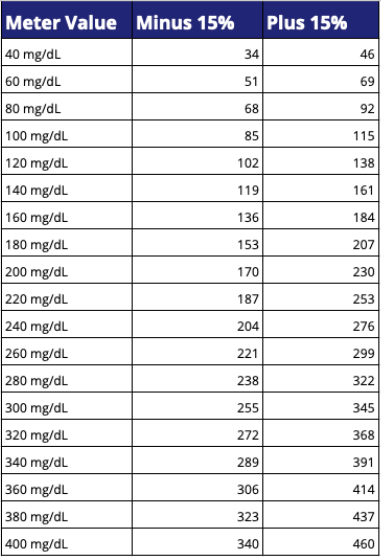
To assess the “variance” in any blood sugar reading of your own, simply multiply the number on your glucose meter by 0.15. Then subtract and add that result to the number on your meter to determine the full range of your actual glucose level.
Example:
211 mg/dL x .15 ≈ 32
211 - 32 = 179 mg/dL
211 + 32 = 243 mg/dL
Could checking again with the same meter help narrow the results to give more accurate readings? Maybe. But realistically, using two or three strips every time you check your blood sugar is not a practical long-term plan. If you’re looking at an extremely high number, checking again might provide a bit more assurance in your calculated correction dose of insulin.
The problem with “variance” in today’s glucose meters
The biggest problem with variance in a blood sugar reading is when people are dosing insulin based on that reading. And 15 to 20 percent of a blood sugar level at 100 mg/dL (according to your meter) means your blood sugar level may actually be at 120 mg/dL or 80 mg/dL. That variance is significant if you’re taking insulin. A ¼ unit of rapid-acting insulin could correct a blood sugar of 120 mg/dL (depending on your correction ratio), bringing it down to 90 mg/dL. Take that same correction when your blood sugar is actually 80 mg/dL, and you’ll find yourself plummeting towards 50 mg/dL.
The higher the blood sugar level, the greater the variance
Now, imagine checking your blood sugar and seeing a 300 mg/dL on the screen.
15 percent of 100 mg/dL is only a mere 15 point accuracy range in either direction, but 15 percent of 300 mg/dL is 45 points. That means your blood sugar could actually be 255 mg/dL or 345 mg/dL. That’s actually a variance range of 100 points.
Now, look at the 20 percent variance of a 340 mg/dL blood sugar reading. It could actually be as high as 408 mg/dL! If you took a correction dose of insulin for 408 when your blood sugar was actually 20 percent lower in the other direction of 340 mg/dL, at 272 mg/dL, you’d inevitably wind up low.
Have you ever taken a carefully calculated dose of insulin to correct a high blood sugar only to find that three hours later your blood sugar is still well over 200 mg/dL? The variance of your glucose meter could easily explain this. You may have taken a correction dose for a blood sugar of 340 mg/dL when you really needed enough insulin to correct a blood sugar of 408 mg/dL.
While this can be frustrating at times, it’s important to keep in mind when making decisions around your blood sugar levels.
Is the same meter consistent in its variance?
Today’s typical glucose meters can produce two different blood sugar levels within even 30 seconds of each other due to variance.
Sometimes, you may find that testing your blood sugar twice in a row only seconds or minutes apart results in fairly similar results -- and other times, with the exact same meter, you could get readings that are different by 20 or 30 points if your blood sugar is high.
Why you shouldn’t use two different glucose meters at the same time
Glucose meter variance is also why it’s important to use only one glucose meter as your primary method of checking your blood sugar. Remember: meters are calibrated to be within 15% of a laboratory result. Not 15% of your previous meter.
If you are using two different brand meters throughout the same day, you’re increasing the degree of inconsistency in your blood sugar results because the variance of one meter might be 15 percent higher than a blood lab measurement and the variance in the other meter might be 20 percent lower.
Since there is no way to avoid variance altogether, the next best thing a person with diabetes can do is use the same meter to help ensure that the degree or direction of variance is more consistent.
The FDA requirements for over-the-counter glucose meters
The FDA’s document on guidance for “Self-Monitoring Blood Glucose Test Systems for Over-the-Counter Use” describes extensive and detailed standards for any glucose meter seeking the FDA stamp of approval.
Here are some details regarding standards for the accuracy and variance of a glucose meter in order to receive FDA-approval.
General accuracy and variance criteria
“Blood glucose test results are used by people with diabetes to make critical decisions about their treatment; therefore, it is important that the results are accurate so that nutritional and drug dosing errors are better avoided,” explains the FDA’s guidance document.
For any glucose meter seeking FDA-approval, studies should demonstrate that 95 percent of all blood sugar level results are within 15 to 20 percent of the blood lab value.
The acceptable 5 percent of results that are greater than a 20 percent variance should be explained in detail by the manufacturer to justify why the errors occurred. Reasons might include an extremely large number of tests or patients using the device incorrectly by not washing their hands before testing, etc.
Accuracy for blood sugars between 50 mg/dL to 400 mg/dL
There is additional leniency from the FDA for blood sugars below or above a certain level.
“The FDA understands that some [self-monitoring blood glucose meters] may not be able to measure reliably within 15 percent of the comparator method at very low glucose concentrations.”
The FDA has deemed 50 mg/dL as the lowest reading at which a glucose meter must be able to measure glucose accurately within the allowed degree of variance.
The upper end of the required accuracy range is 400 mg/dL.
To receive FDA-approval, a glucose meter must present an error code (or the words “HIGH” or “LOW”) for blood sugar levels below 50 mg/dL or above 400 mg/dL if the meter is not able to accurately measure those levels.
Why aren’t glucose meters 100 percent accurate?
You might be wondering why the FDA doesn’t tighten their standards. Unfortunately, there are a variety of factors that account for that acceptable variance range. Here are some of the many variables that impact the exact accuracy of your glucose meter results, according to a study published in the Journal of Diabetes Science and Technology, funded by Wavesense Technology.
Enzyme vulnerability & consistency
Enzyme vulnerability refers to several variables and environmental issues that can be inconsistent when you’re checking your blood sugar. Some you have control over, others you don’t.
For instance, when a test strip is created in the manufacturing plant, a reactive enzyme is sprayed across the inner page of the test strip, then other details of the strip technology are added. When your blood is applied to the strip, it reacts with that enzyme as a key part of producing a blood sugar result. If the test strip material wasn’t covered thoroughly in the enzyme spray, it can affect the accuracy of your results.
Other environmental variables include things like how the strips are stored, the conditions they endure during shipping, whether they are kept in an extremely hot and humid area versus cold and dry, and so on.
While the manufacturers of test strips generally have highly controlled storage environments for their product, they can’t control these details once the product ships and shows up at your door or at the pharmacy.
Capillary blood vs. venous blood
The blood in your capillaries (which are in your fingertips) is not identical to the blood in your veins. While they are very close according to research, they are rarely the same.
When compared to a blood draw in a lab, where the blood is always taken from a vein in your arm or hand, at a controlled temperature, in an extremely sanitary and enclosed tube, and then assessed in a very controlled lab, it’s actually not surprising that at-home glucose meters aren’t able to produce an exact measurement.
This is similar to the reason the results on a continuous glucose monitor (CGM) do not exactly match your blood glucose meter. CGMs measure the glucose in your body’s interstitial fluid -- the fluid in your bodily tissue -- not the glucose in your bloodstream. The glucose in your bloodstream actually reaches your interstitial fluid about 15 minutes after it is pumped through your bloodstream. If your blood sugar is trending upward or downward, the CGM and capillary glucose meter numbers could and should be quite different.
Your hydration level
Did you know that even mild dehydration can have a pretty significant impact on your blood sugar level?
Dehydration can result from any number of regular events in life, any of which can impact your blood sugar levels:
-
Intense exercise
-
Not drinking enough fluid during the day
-
Consuming an excessive amount of sodium and/or potassium
-
Excessive sweating
-
Coffee and other caffeinated beverages
-
Alcohol
-
Air travel
-
Certain medications (diuretics, Invokana, etc.)
-
Menstruation
-
Mental / emotional stress
-
High altitudes
-
Diarrhea
-
Vomiting
-
Hot, humid weather (Florida)
-
Hot, dry weather (Arizona)
-
Breastfeeding
-
Old age
Getting enough water in your day as a person with diabetes is critical! Not only for meter accuracy but for your blood sugar levels and your overall well-being.
* Personally, I’ve seen this during a bout with the norovirus. After vomiting more than 10 times in a row -- clearly depleting my body of necessary fluid and becoming instantly dehydrated -- I watched my blood sugar soar from a normal 100 mg/dL to nearly 400 mg/dL over the course of an hour. However, after just 1 hour of starting intravenous saline with electrolytes at the hospital, my blood sugar according to my glucose meter came back down below 200 mg/dL on its own.
That’s why it’s so important to get to the hospital if you are vomiting repeatedly and can’t keep your body hydrated as a person with diabetes.
Glucose distribution in one drop of blood & different sites
Related to your body’s hydration level, the amount of glucose in that one tiny drop of blood applied to the test strip can vary slightly. Had you squeezed out another drop from the same finger 30 seconds later, it could contain a modestly different amount of glucose.
On the same note, the glucose in the blood sample from your fingertips versus the glucose in your forearm or earlobe (where emergency medics often draw from) can also vary.
If you are using a glucose meter and lancing device that allows you to draw blood from your forearms in addition to your fingertips, keep this in mind. Constantly switching between alternate sites like your forearm and fingertips could produce inconsistent results that inevitably make your insulin dosing inconsistent, too.
How you prepare (or not) before pricking your finger
Especially among children (and likely amongst adults, too), studies have found people with diabetes rarely wash their hands prior to glucose testing. Even if you weren’t recently touching food -- something that could easily lead to an inaccurate reading -- other things on your hands could potentially affect the accuracy. Hand lotion, ink from a newspaper, hair product, make-up, sweat, and even water after washing your hands if you don't dry them thoroughly.
Proper blood sugar checking technique for greatest accuracy:
- Wash your hands or use an alcohol swab on that finger (allow to dry thoroughly)
- Be sure your test strips are within their expiration date
- Use control solution to verify your strips and meter are reading within range
- Avoiding touching the end of the strip where blood will be applied
- Be sure to apply enough blood to completely fill the test strip
- Avoid testing in extremely hot or cold temperatures
- Be sure to completely close the test strip container to prevent humidity and other environmental factors from negatively impacting all of your strips
In real life diabetes management with type 1 diabetes or type 2 diabetes, it’s not always possible to control all of these variables. But keep in mind that if you’re checking your blood sugar at the top of a mountain in New Mexico and your entire diabetes kit feels hot to the touch, your results may not be as accurate. The same goes for checking in the middle of a ski trip to Vermont when it’s 10 degrees outside!
Affordable, accurate, unrestricted
If you’re tired of your health insurance telling you how many times per day you’re able to check your blood sugar then rest assured, you have options. Diathrive’s glucose meters provide accurate results for a fraction of the cost, and without limitations. Get as many tests trips as you want so you can use blood sugar results to make health decisions whenever and wherever you want in real-time.
At Diathrive, accuracy is extremely important, and we've made sure our meter meets and exceeds FDA standards. Our mission is to help you check as often as you need to for the sake of managing and improving your diabetes health!






